A biomedical engineer, passionate Researcher and curious mind, Mattia Ballerini embarked on a path that took him from the Politecnico di Milano to the laboratories of the European Institute of Oncology, combining engineering, mechanics and biotechnology.
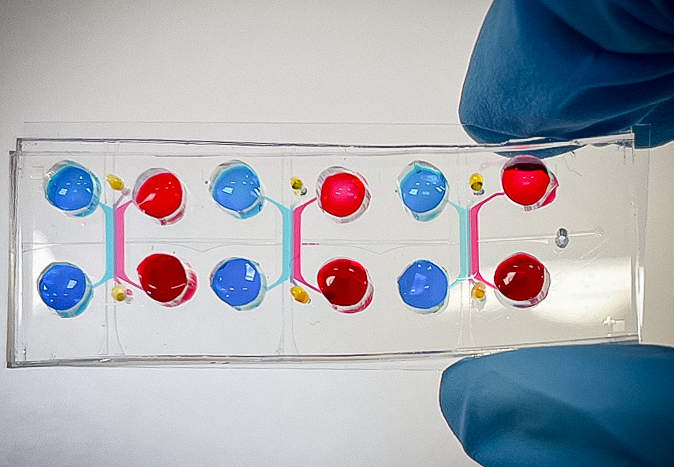
What is the core work he carries out? Organs-on-chip, miniature devices capable of mimicking the functions of actual human organs. They are created in the laboratory to study complex diseases and to test therapies in a more realistic, safe and effective way.
In this article Mattia takes us behind the scenes of his project — gut-on-chip— showing us how two seemingly distant worlds, such as engineering and medicine, can create technologies capable of responding, with their great impact, to the health challenges of the future.

Mattia, let’s start with you. Tell us something about the path you followed.
I spent my entire academic career at the Politecnico di Milano, starting with the BSc in Biomedical Engineering, and continuing with a MSc, always in the same field. I specialised in Biomechanics and Biomaterials (BBB), a track with a strong focus on mechanics. However, over time my interest shifted to more cellular issues related to microfluidics.
During the three-year bachelor’s degree programme, I had already begun to explore these issues with a dedicated thesis. The Master’s degree programme offered me the opportunity for in-depth study by working at the MiMic Lab, where I developed an automated system for crop control in microfluidic devices.
The partnership with the European Institute of Oncology, established by Dr. Luigi Nezi, marked a turning point in my career. That was where the opportunity to pursue a PhD came from. Indeed, the project I am still working on today was conceived in that context.
How did the idea of using a “gut-on-chip” model to study the response to immunotherapy in melanoma come about?
The convergence of different skills and visions acted as a trigger. Dr. Luigi Nezi, now Group Leader of the IEO’s Department of Experimental Oncology, came from an experience in Houston, where he had worked on gut microbiota using in vivo models. On returning to Italy, he wanted to explore alternative approaches that would allow him to work on systems based on human cells, while maintaining the structural and functional complexity typical of an organ. This is where the gut-on-chip comes in.
Organ-on-chip technology, on which Prof. Marco Rasponi, Head of MiMic Lab at Politecnico di Milano, has long-standing experience, seemed to offer the right balance with the concept of a three-dimensional human model, reproducible and suitable for simulating realistic physiological conditions. The project was conceived from this synergy between bioengineering and oncology.
What was the idea behind it?
The idea was to develop a device capable of faithfully reproducing the human gut environment in order to investigate the role of microbiota in the response to immunotherapy in patients with melanoma. This is a central issue today, more than ever, as the microbiota has proven to be a key player not only in daily health, but also in many pathological conditions, including cancer.
The project was an instant success. We developed a working model able to support the experimental hypothesis and reproduce in vitro the key conditions for studying the interaction between gut microbiota and immune response in cancer patients.
We have put a great deal of effort into this project, driven by a strong motivation towards a topic that we feel is particularly close to our heart, and this constant dedication paid off last February, when the main results of our research were published in Nature Biomedical Engineering, confirming the value of the path we have taken.
Can you explain in simple words how the “gut-on-chip” works?
We started with an existing device at the MiMic Lab. It was initially designed for the heart-on-chip. Despite differences in terms of purpose, the geometry was consistent, so we adapted the design to simulate the gut.
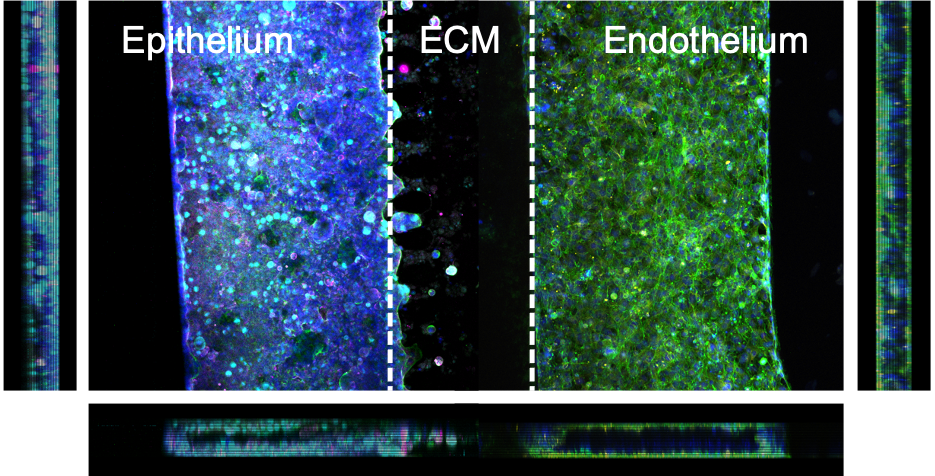
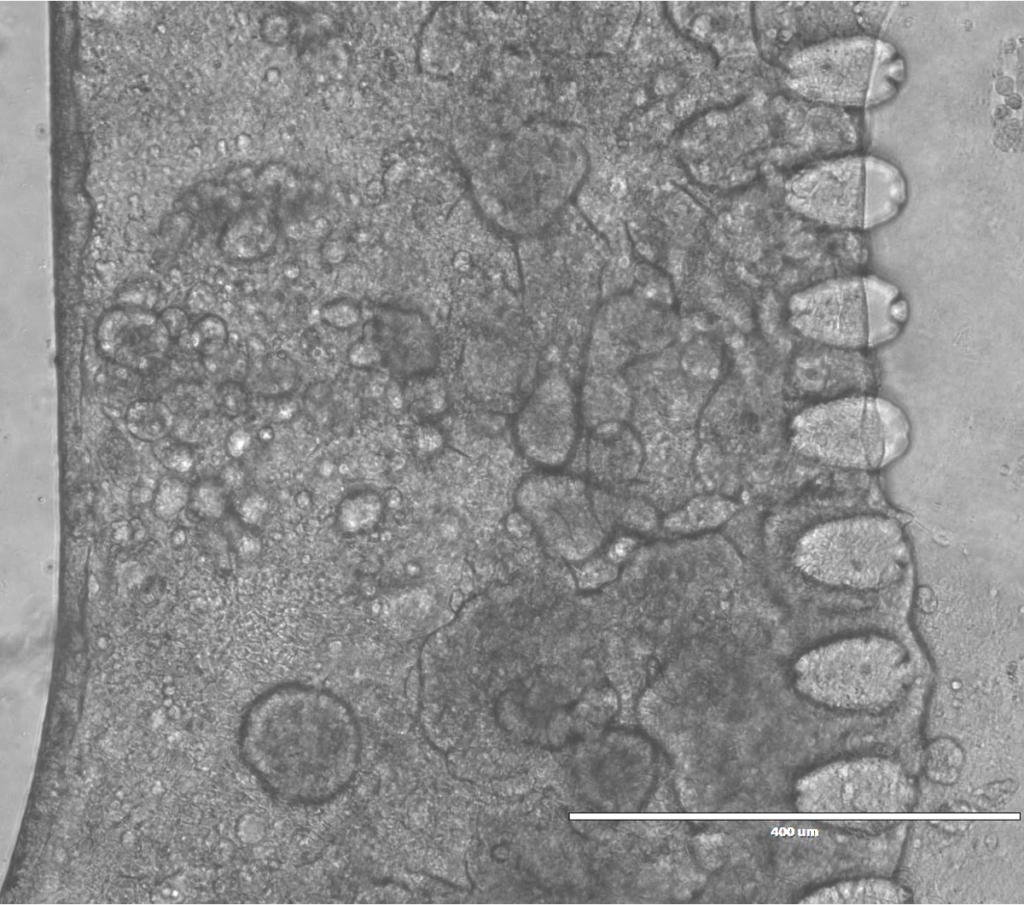
The main objective of the gut-on-chip is to recreate not only the architecture, but also the dynamic functions of the human gut. We focused on the intestinal epithelium, which is the first barrier in contact with the microbiota, the bacteria, viruses and fungi that live in our intestines and play a crucial role in both the state of health and the progression of many diseases.
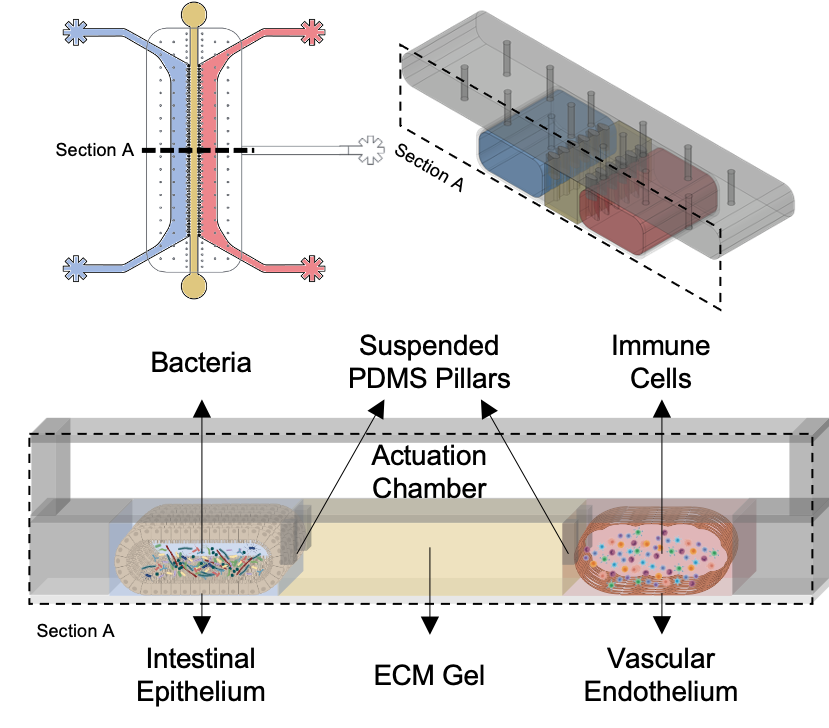
In the device we recreated this intestinal barrier by using human cells, to which we also added a vascular component, to simulate immune responses and observe any systemic effects.
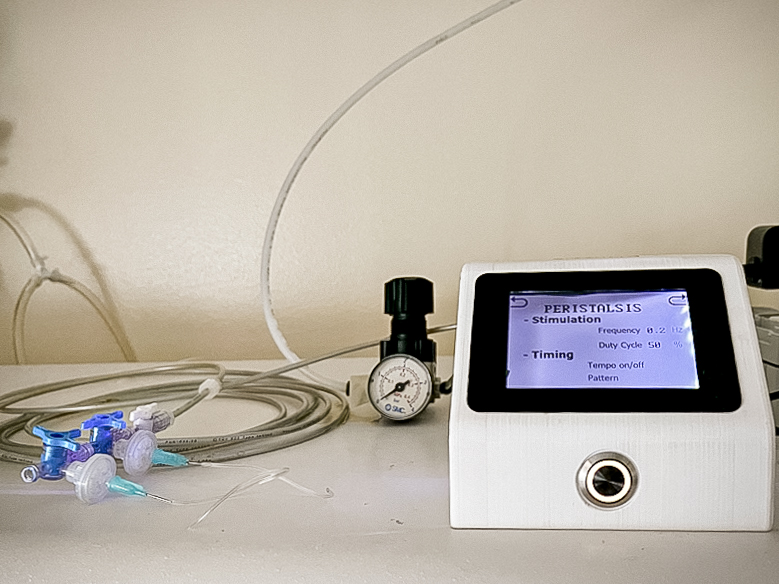
A key element was the insertion of mechanical stimulation to mimic the peristaltic movements of the gut. This dynamic proved to be crucial. In static conditions, cells grow less and present a flat layout. When stimulated, they form more complex and realistic structures, such as typical intestinal villi, and produce more mucus, an essential condition for a balanced interaction with the microbiota.
In your study, you identified a link between the composition of gut microbiota and the efficacy of immunotherapy in patients with melanoma. What does this discovery mean in clinical terms?
We performed a series of co-culture experiments by modelling both human intestinal cells and microbiota samples taken from patients. What we observed was that the microbiota of healthy donors or patients who responded to treatment maintained the intestinal barrier intact, while that of patients who did not respond to immunotherapy caused a breakdown of the barrier and marked inflammation, which also spread to the vascular compartment, activating a dysfunctional immune response.
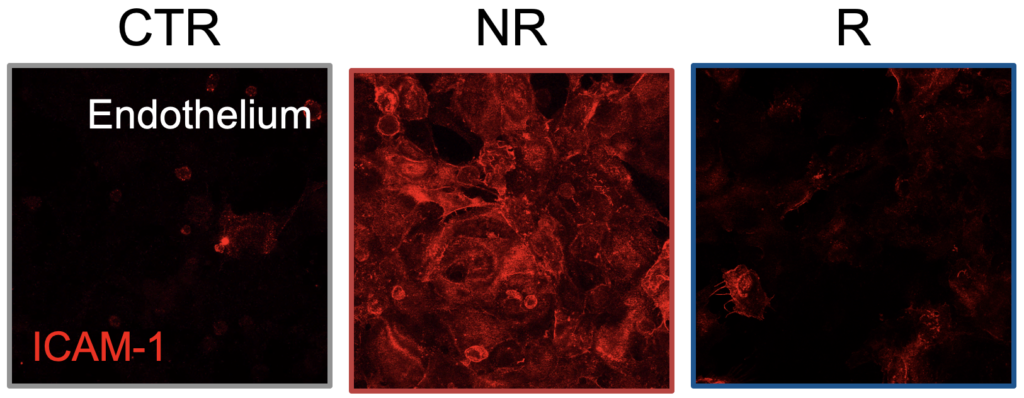
In selected cases, we also tried to modulate the microbiota of non-responder patients — for example, by combining it with responder microbiota. In these cases we saw a reduction in inflammation and an improvement in local response. These results suggest that, in the future, we could use devices like ours to test a patient’s response to different therapies before even administering them, or even to manipulate the microbiota and “prepare” the patient for therapy.
Do you think this model could extend to other organs or diseases in the future?
Yes, and it is something we are already actively working on. uBeat technology, on which our gut-on-chip model is also based, aims to integrate a dynamic environment into organs-on-chip, i.e., one that can simulate the mechanical stimuli — such as heartbeat, respiration or peristalsis — that are essential for proper tissue function in the human body.
We started from the heart, and today we are already adapting uBeat for other organs. For instance, we are applying it to the joints, to simulate the mechanical movement of cartilage during walking or physical activity, or to the lungs, where breathing is a key element. Of course, we also applied it to the gut to reproduce peristaltic movements. Every time we introduce dynamic stimulation, we observe a more realistic and physiologically significant cellular behaviour.
Another very interesting line of development, which we are currently exploring, concerns multi-organ models. We are creating devices that allow different organs, such as heart and liver, to communicate to study complex phenomena such as cardio toxicity linked to hepatic drug metabolism. Once again, uBeat technology plays an essential role in these models.
Finally, we are working on an even more ambitious evolution, precisely personalisation of the model by adapting uBeat to the characteristics of the individual patient. This is particularly important, for example, in cardiac models derived from stem cells, which often do not reach a level of maturation equal to that of the adult heart in vitro. The idea is to calibrate mechanical stimulation specifically to obtain organs-on-chip that increasingly mirror human physiology.
Today there is much talk about the integration of engineering and medicine. In your opinion, how important is this collaboration for the development of more effective and less invasive therapies?
I believe the integration of bioengineering and medicine is essential to really push research forward. Although these two disciplines still follow parallel tracks in some areas today, there is a growing openness and willingness to collaborate, especially in more interdisciplinary contexts.
In my case, during my PhD, I mainly worked at the European Institute of Oncology, where I was in close contact with biologists, biotechnologists, etc. I was often the only engineer in the laboratory — and almost even in the entire institute [he laughs] — but despite this the interaction was always positive. Everyone brought their skills to the table, and sharing ideas led to more complete and effective solutions.

It is clear that certain applications require very specific knowledge, and only a genuine dialogue between experts from different fields can build something useful and innovative. Working together has also greatly enriched my personal know-how. By cooperating with people from a different background, I learnt new things, and was able to overcome challenges, achieve goals and contribute more concretely to the project.
So, I would say yes, collaboration is important. Indeed, it is indispensable, if we want to do research that has a real impact.
Personally, what did this project leave you?
The PhD has been an intense process, lasting four years. As often happens, at first you come up against more failures than successes. It is a phase in which we learn not to be discouraged, to look for the positive aspects even when results do not come immediately. And it is not always easy.
But what never failed was my enthusiasm for what I was doing. I was aware that I was in a stimulating environment, working on research I was passionate about. This pushed me to overcome difficulties. Every obstacle was a challenge to be understood and solved, not a reason to stop. Finally, the results arrived with a great deal of satisfaction.
Another very important aspect has been the continuous interaction with people from different backgrounds—engineers, biologists, doctors. Comparing notes with them allowed me to grow considerably not only in terms of know-how, but also on a personal level. Moreover, knowing that our work can have a real impact on patients’ lives makes it more meaningful. It is a piece in a larger puzzle, but knowing it can be useful, tangible, real, enhances motivation.
Looking ahead: what are your future ambitions?
I have currently returned to the Politecnico di Milano as a post-doc, and I am continuing my work at the MiMic Lab, always focusing on organ-on-chip technology. I am very passionate about this area, also thanks to the stimulating and collaborative environment of the laboratory, where daily discussions with colleagues makes the work even more rewarding.

In the future, I do not exclude the possibility of exploring new avenues, such as different applications or similar applications but more at the corporate level. What interests me is to continue doing research. Whether in an academic setting or in a more corporate context, I would like to remain connected to this world, with all its merits and challenges.
For now I have no precisely defined projects, but I am using my time at the Politecnico to expand applications of the technologies I work on, while also growing both personally and professionally. The goal is to continue learning, experimenting and contributing to the development of innovative solutions, perhaps in unexplored areas.
