The HyperSKIN project, an innovative device for diagnosis and treatment of non-melanoma skin cancer, has just been awarded a grant from ERC, the European Research Council. The 18-month ERC Proof of Concept 2024 grant will be used to finance the technical and commercial feasibility study in order to move on to the next stage, which is marketing the device.
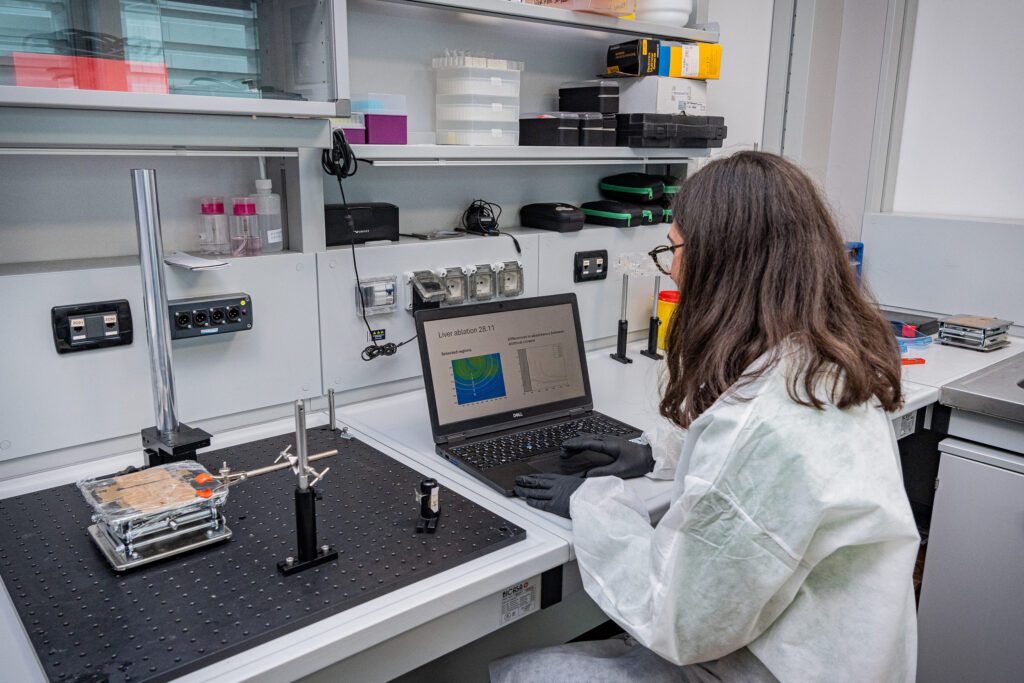
We met with Paola Saccomandi, research team lead at the Lambda Lab (Laboratory of Measurements for Biomedical Applications), Department of Mechanical Engineering, Politecnico di Milano, to explain how HyperSKIN works. The aim is to develop a contactless device «that can assist the decision-making process, both before and during surgery, in accurately establishing tumour margins. It provides instant feedback on which skin regions to preserve and which to remove, thus acting as a digital biopsy».

By refining light-based treatments for non-melanoma skin cancers (NMSC) through optimisation of laser light settings, the system will define a solution without collateral damage, with minimal damage to surrounding healthy tissue, rapid procedure times, and high standard clinical results.
It is a hot topic. According to data provided by GLOBOCAN, the Global Cancer Observatory of the International Agency for Research on Cancer, World Health Organisation (WHO), there were 1,234,533 new cases of NMSC globally in 2022, of which 330,062 in Europe (approx. 26.7%). The most common causes of onset, besides the age factor, are, of course, exposure to UV radiation, but also to chemicals such as arsenic.
How does the HyperSKIN system work?
«There is an initial phase in which a kind of fingerprint of the NMSC is obtained by acquiring images through a hyperspectral camera. It is not the typical photograph that corresponds to the colours we normally see. Indeed, it also includes information that falls within the non-visible spectrum. The various images correspond to different wavelengths, and a classification is then made on the basis of the tissue biomarkers identified, i.e. the characteristics that distinguish normal and tumour tissues. Based on this information, the system recognises a tumour and what is not a tumour. The margins of the neoplasm can thus be identified more accurately. At this point, the tumour can be directly treated with a laser light».

So this system would also allow cells around the visually evident area, which are perhaps more spaced out and isolated, to be removed as much as possible?
Exactly. One of the main problems with skin cancers is to precisely define the margin. If cancer cells remain, there is a risk of recurrence. These cells cannot always be identified with current diagnostic techniques because they behave differently visually».
Focus is on non-melanoma skin cancers. Can you explain why?
«In terms of clinical procedure, laser treatment, which burns the skin, cannot be performed when there is a melanoma as the surgeon would not be able to take tissue for diagnosis and staging of the malignancy. Laser light with optimised intensity and no risk for the patient could, instead, be an option for non-melanoma, which is a superficial and localised cancer. It is much more frequent but also less dangerous than melanoma. We hope that, some time in the future, the HyperSKIN system may also be applied for the diagnostic and post-operative phase of melanoma».
Can we say that HyperSKIN is the outcome of an earlier project headed by the Politecnico di Milano, and funded by the ERC?
«Yes, it developed in the wake of the Laser Optimal project for intraoperative monitoring of light-based cancer treatment. The part where we studied how hyperspectral imaging evaluates thermal damage caused by laser light was funded by an ERC Starting Grant, and led to this and other projects».
